9F, Zhongrui Jumei Building, 68 Jiuzhang Road, Suzhou Industrial Park, Jiangsu Province
Medical information
A new study has found the presence of antibo-producing B cells in the turbinate that defend against microbial invasion through the nose
The nose is the main gateway to our bodies - the air we breathe, the aromas we smell, and the microbes that make us sick all enter our bodies through it. When the air enters the nasal cavity, it passes through the turbinate conchae - a long, narrow, curled skeleton that looks like a shell protruding from the breathing passages.

The turbinate is covered by a unique tissue that secretes mucus and contains many branches of nerve cells responsible for the sense of smell. The structure and function of the turbinate allows air to warm up and absorb moisture before it reaches the lungs.
Not only is the turbinate a major site for pathogens to enter the respiratory tract, it is also a major weak link: Because the turbinate is so close to the brain, our immune system is unable to release antibodies to it through the bloodstream during an upper respiratory infection. So, how do we protect ourselves from microbes invading through the nose without getting sick so often?
In a new study, researchers from the Weizmann Institute of Science have found that whenever we are sick or vaccinated, antibot-secreting cells migrate to the turbinate and from there secrete antibodies locally into the nasal cavity. The discovery could pave the way for more effective nasal vaccinations and the development of new therapies to treat neurological disorders, allergies and autoimmune diseases. The results were published online July 31, 2024, in the journal Nature ina paper titled "Turbinate-homing. IgA-secreting cells originate in the nasal lymphoid tissues ".
During the coronavirus pandemic, as the virus spread across the globe, millions of people kept a close eye on what could be delivered via a nasal spray rather than an injection COVID-19 vaccine development. The idea is not outlandish; After all, flu vaccines and several other vaccines are already available through nasal sprays that contain live attenuated viruses that confer local protection in the turbinate.
However, this type of nasal vaccine is not effective with a single dose and must be followed by a booster dose. However, scientists still don't fully understand how these types of nasal vaccines work and why booster shots are needed.
To figure this out, Professor Ziv Shulman of the Weizmann Institute of Science's Department of Systems Immunology and doctoral student Jingjing in his lab Liu decided to study how the immune system organs near the nose and throat respond to the nasal vaccine. In humans, these organs include the tonsils and adenoids, collectively known as Waldeyer's lymphatic ring (Waldeyer' s lymphatic ring (Waldeyer' s tonsillar ring).
In the new study, the research team used advanced imaging techniques to analyze the body's immune response by imaging complete immune system organs in mice, similar to those in humans. They found that when mice were vaccinated with the nasal vaccine, the main antibody producer in the immune system -B The cells produce a concentrated immune response. These cells begin their journey with precursor B cells, some of which have the potential to recognize pathogens.
The team saw how cells close to mucosal tissue in the nasal cavity recognized the vaccine molecule and began to rapidly divide and differentiate. This process of differentiation can be seen as a process of biological specialization, which ends when they become cells that secrete specific antibodies against pathogens or become memory cells. Memory cells can be stored for a long time to prepare for future infections.
B cells can secrete five types of antibodies. The team found that after vaccination, B cells close to the nasal cavity change the identity of the antibodies they produce and start secreting antibodies that function like goalkeepers and specifically enter the nasal cavity from the internal mucosal tissue.
The next stage is B The cells move from their location near the nasal cavity to the tiny "training camp," the germinal center, which is located in the immune system organs in that part of the body. Once there, they are "trained," including altering their genetic makeup and carefully selected to ensure that only those that produce antibodies effectively correlate with the pathogens the vaccine targets B cells to survive.
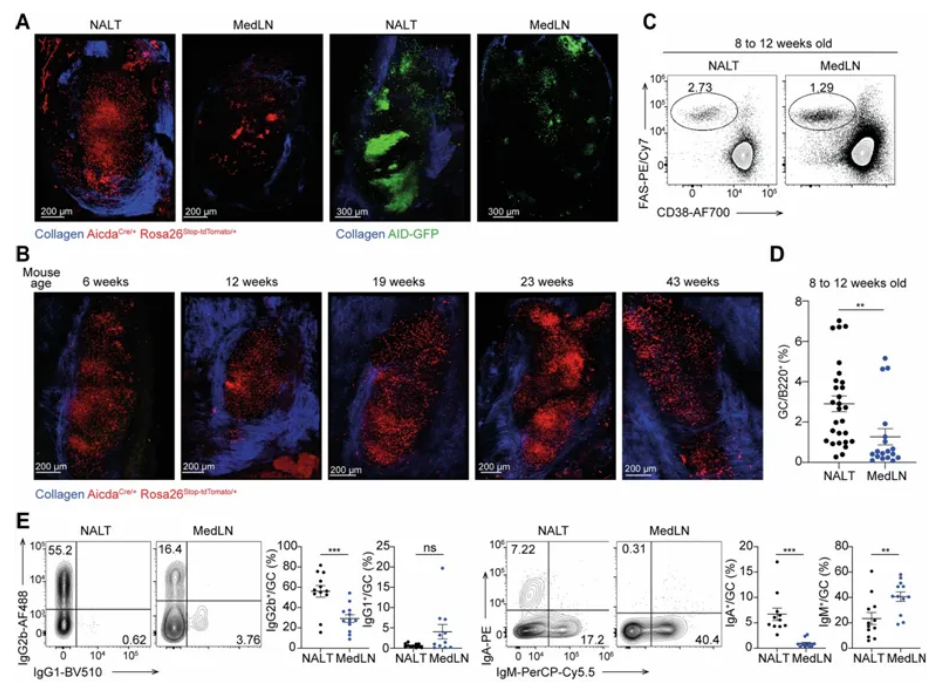
Image from Nature, 2024, doi:10.1038/s41586-024-07729-x
In this training program, the B cells were helped by a certain type of T cell that even played a role in determining which cells ultimately survived, but the team found that there were not enough T cells in the immune system organs in that part of the body to produce an effective immune response.
Shulman explains, "The fact that T cells have to migrate to this area explains why one dose of the nasal vaccine is not enough and a booster vaccination is needed." Only after a second dose of the vaccine is sufficient to be produced T cells, thereby transforming B cells into effective antibody-producing and memory cells."
The research team believes that T The scarcity of cells is to prevent over-sensitivity to harmless foreign objects in the air. Shulman added, "This mechanism can be problematic when people develop allergies and various autoimmune diseases, so understanding this mechanism could help develop new ways to treat these diseases."
Immune treasure hunt
The discovery that this immune mechanism is activated in response to a vaccine is just the starting point for an in-depth quest to determine where antibody-secreting cells go after completing the differentiation process.
"We visualized the immune response in the nasal lymph nodes, but how does that translate into airway protection? We were surprised to find that B The cells are present in the turbinate, and this bone tissue is not known to support antiboy-mediated immune responses. This migration to bone tissue is similar to what happens in the bone marrow, and it's possible that this niche environment plays other roles in addition to this immune mechanism that we found."
These new findings suggest that these antibody-producing cells move from the nasal lymph nodes to mucus-producing glands in the turbinate, directly below its outer layer of cells, and secrete the antibodies into these glands. This immune defense function compensates for the inability of blood antibodies to enter this channel through the bloodstream, and it is not only important in viral infections and other diseases: it also protects many nerve endings in that part of the brain and body, which are responsible for our sense of smell.
In addition to facilitating vaccine design, Shulman noted that the study exposed "entry points into highly fortified targets - antibody-secreting cells that can enter the central nervous system." In the future, it may be possible to use antibody-secreting cells to enter the olfactory nerve to design vaccines against neurological diseases.
Reference: Jingjing Liu et al. Turbinate-homing IgA-secreting cells originate in China the nasal lymphoid tissues. Nature, 2024, doi:10.1038/s41586-024-07729-x.
Source: Bioon Cells

