9F, Zhongrui Jumei Building, 68 Jiuzhang Road, Suzhou Industrial Park, Jiangsu Province
Medical information
Nature: After recovery, the patient still suffers from immune deficiency. What did COVID-19 do to B cells?!
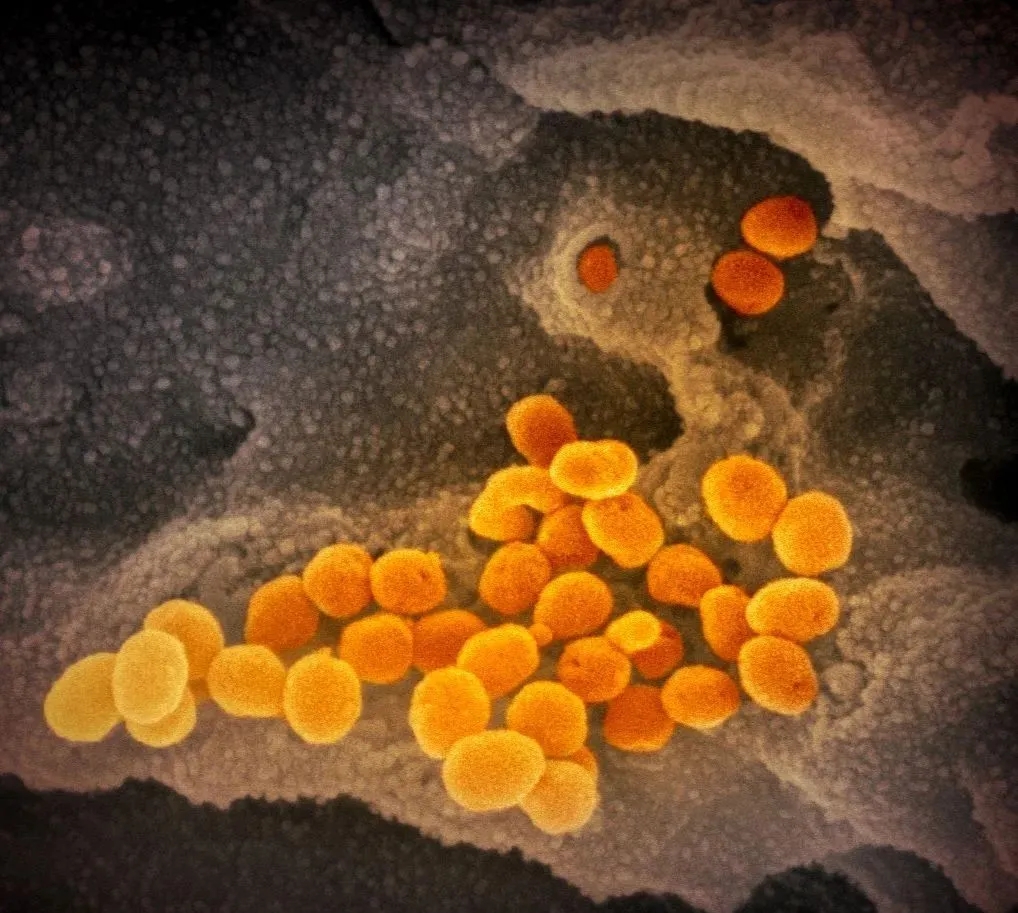
At the end of 2019, a new novel coronavirus (SARS-CoV-2) was confirmed as the pathogen of COVID-19 severe acute respiratory infection. The clinical manifestations of patients with SARS CoV-2 infection vary widely, ranging from asymptomatic to life threatening severe cases, including acute respiratory distress syndrome (ARDS). The so-called "cytokine storm", which refers to the uncontrolled activation of inflammatory reactions, significantly promotes the occurrence of ARDS. Similar to other diseases that trigger cytokine storms, suppressing inflammatory immune responses may improve the outcome of severe SARS CoV-2 infection
Current evidence indicates that serum metabolic components in COVID-19 patients have significantly changed compared to healthy individuals, and are associated with disease severity. The metabolic environment, such as changes in glucose concentration, access to short chain fatty acids, and oxygen supply, affects the survival, activation, and differentiation of B cells. Therefore, the specific metabolic environment in COVID-19 patients may change the biology of B cells, and B cells also play a variety of roles in the progression of COVID-19 disease
The purpose of this study was to evaluate the signal characteristics of B cells from COVID-19 patients and determine how changes in the abundance of specific metabolites affect B cell receptor signals by analyzing serum metabolic components obtained from COVID-19 patients
SARS-CoV-2 infection alters the immune phenotype and B-cell function specific subsets of convalescent patients, which play a key role in antiviral humoral immunity. In order to investigate whether SARS-CoV-2 infection affects the immune phenotype of B cells, we first tested immature B cells (CD27 IgD+), atypical (CD27 IgD -), switched (CD27+IgD -), and unshwitched (CD27+IgD+) memory B cells, transitional B cells (CD38+CD24hi), and seroplasma cells (PBC, CD38+CD24 −). During the resting phase, the healthy control group and the rehabilitation patients had similar B cell populations, but the frequency of PBC in patients increased significantly compared to the healthy control group. To detect the response of B cells to bcr dependent signals, we stimulated B cells with F (ab ') 2 anti human Ig (M+G) antibodies for 24 hours. However, compared to the resting state, the number of atypical memory B cells increased (Figures 1a-e). Compared to the resting state, the frequency of stimulated non switched memory B cells in patients decreased, but there was no change in the healthy control group (Figure 1a, c). Interestingly, the expression of CD19, a key regulator of the BCR signaling pathway, was significantly reduced in total B cells and almost all B cell subsets in rehabilitation patients compared to healthy controls (Figure 1f). However, compared to the healthy control group, there was no change in CD19 mRNA expression on B cells in rehabilitation patients (Figure 1g). Immunofluorescence experiments showed that the expression of CD19 in the spleen of SARS-CoV-2 infected mice was significantly reduced compared to uninfected (simulated) mice (Figure 1h, i). These results suggest that SARS-CoV-2 infection may alter the immunophenotype and function of B cells by inhibiting the expression of CD19
SARS-CoV-2 infection alters BCR signaling and b-cell metabolism in convalescent patients. CD19 is a key regulator of BCR signal transduction, b-cell development, and humoral immune response. Compared with the healthy control group, the levels of total CD19, phosphorylated CD19, and phosphorylated Btk in patients' B cells were significantly reduced (Figure 2a). CD19 is an important activator of the PI3K signaling pathway in anti ig (M+G) stimulated cells. When detecting the activation of PI3K and its downstream signals by anti ig (M+G) stimulated B cells, phosphorylated PI3K, Akt, FoxO1, S6, and mTOR in patient B cells were significantly reduced compared to healthy controls (Figure 2b). Since PI3K signal is the main regulator and redox signal of b cell metabolism, we speculate that SARS-CoV-2 infection alters b cell metabolism. Abnormal production of reactive oxygen species (ROS) can lead to impaired survival of normal and germinal center B cells, and mitochondrial ROS inhibits humoral immune responses. Compared to untreated patient B cells, levels of CD19 and pBtk on antioxidant treated patient B cells were significantly increased (Figure 2c). To evaluate the redox status of B cells from COVID-19 patients, we stimulated B cells from patients and healthy controls with F (ab ') 2 anti human Ig (M+G) to determine total ROS production. The results showed that patients' B cells produced more ROS than healthy controls (Figure 2d). Mitochondrial complex III is necessary for hypoxia induced ROS production and cellular oxygen sensing. Compared to healthy controls, mitochondrial swelling in patient B cells increased (Figure 2e). Endoplasmic reticulum (ER) homeostasis is maintained by regulating mitochondrial calcium levels to shape b cell metabolism and metabolic stress responses. Compared with the healthy control group, the MFI of ER and MITO in patients' B cells significantly increased at 0 and 5 minutes, but decreased at 30 minutes (Figure 2f-i). In addition, compared to the healthy control group, the co localization between BCR and ER or MITO was significantly reduced during the entire b cell activation process (Figure 2j k). We also found that the co localization of ER and MITO in patients' B cells significantly decreased at 0, 5, and 30 minutes compared to healthy controls (Figure 2l). These results suggest that SARS-CoV-2 infection may alter the metabolic activity of b cells and increase ROS production, thereby reducing CD19 expression and bcr dependent signal transduction
3. SARS CoV-2 infection changed the serum metabolite profile and transcriptome profile of B cells. The levels of l arginine, l glutamic acid, l isoleucine, l cystine and l cysteine in the serum of patients with COVID-19 rehabilitation were significantly reduced. Compared with the healthy control group, the levels of glutamic acid and cysteine in the serum of convalescent COVID-19 patients were significantly reduced. Detect the difference in B cell transcriptome between convalescent COVID-19 patients and healthy control groups, and find that compared to healthy control groups, 48 gene expressions are significantly decreased and regulated, while 10 gene expressions are significantly upregulated (Figure 3f). KEGG functional enrichment analysis revealed that a total of 20 pathways were enriched in differentiation genes/metabolic genes, most of which were metabolic signaling pathways, especially amino acid synthesis and metabolism (Figure 3g). Finally, using KEGG to identify the metabolic pathways of genes and metabolites, it was found that there were significant differences in 30 metabolic pathways between healthy control groups and rehabilitation patients (Figure 3h). In the transcriptome, the longevity regulatory pathways - multispecies, biosynthesis of valine, leucine, and isoleucine, biosynthesis of neomycin, kanamycin, and gentamicin, carbon metabolism, and estrogen signaling pathways are highly enriched (Figure 3h). In the metabolic group, purine metabolism and carbon metabolism are highly enriched (Figure 3h). Correlation analysis was performed on the genes and metabolites detected in each differential grouping, and Pearson correlation coefficient> 0.8。 The above results suggest that SARS-COV-2 may alter b cell metabolism through these pathways. In summary, SARS-CoV-2 infection may affect the BCR signaling pathway by altering the metabolic and transcriptome profiles of B cells
SARS-CoV-2 infection alters the BCR signaling pathway by affecting the early activation of B cells. In terms of B cell proliferation, compared with primitive B cells and memory B cells in the healthy control group, the contact area of patients' initial B cells decreased after 3 minutes of activation, and the contact area of patients' memory B cells significantly decreased after 5 minutes of activation (Figure 4a-c). For total BCR signals, the MFI of pY in patients with uninfected B cells and memory B cells significantly decreased at 3 and 5 minutes compared to uninfected B cells and memory B cells in healthy control groups (Figure 4a, B, d). Compared to naive B cells and memory B cells in the healthy control group, the MFI of BCRs decreased significantly at 3 and 5 minutes (Figure 5a-c). In addition, compared to uninfected B cells and memory B cells in the healthy control group, the MFI of pSHIP was significantly reduced 5 minutes after activation of uninfected B cells and memory B cells (FIGS. 5a, B, d). For CD19 activation, MFI of pCD19 in uninfected and memory B cells in patients significantly decreased at 3 and 5 minutes compared to uninfected and memory B cells in healthy controls (Figure 6a-c). These results suggest that SARS-CoV-2 infection alters the BCR signaling pathway by inhibiting the early activation of naive B cells and memory B cells
Through transcriptome and metabolic studies, this study found that gene expression disorders related to metabolism and metabolites, and increased ROS in B cells in rehabilitation patients, indicating an increase in B cell metabolism in rehabilitation patients. Interestingly, the use of antioxidants can partially salvage CD19 expression in convalescent patients. In addition, we found that the expression of CD19 in the spleen of SARS-CoV-2 infected mice also decreased, or it may be thought that the expression of CD19 may also decrease in infected patients. Detecting the expression of CD19 and the metabolic status of B cells in patients with mild and severe infections deserves attention. In addition, the correlation between CD19 expression and different metabolic states of B cells is worth studying. More exciting is that correcting the increased ROS in B cells saves the expression of CD19 and BCR signals, which may correct the immune status of convalescent patients. It is currently unclear whether convalescent patients with reduced CD19 expression are more likely to be re infected with SARS-CoV-2. If this is true, metabolic modulators such as NAC have the potential for clinical use in preventing secondary infection in convalescent patients. Although a decrease in CD19 expression was found, there was no change in CD19 mRNA levels in B cells from convalescent patients, indicating that SARS-CoV-2 infection may have reduced the level of CD19 expression during the post transcriptional translation period. We also detected several molecules in the BCR signaling pathway from RNA-Seq, but did not find any differences in CD19 mRNA and molecules in the BCR signaling pathway between healthy controls and patients. This may be the reason why the BCR signaling pathway does not appear in KEGG enriched signaling pathways. Bacterial and fungal infections are common complications in patients with viral pneumonia and lead to increased mortality. Analyzing the signal characteristics of B cells in COVID-19 patients can help assess whether COVID-19 infection makes patients more susceptible to other diseases, and can better understand how metabolic abnormalities in patients' serum affect B cell signals, which may inspire the development of new treatment strategies for specific metabolic pathways. Different compounds that alter cell metabolism and redox status are currently being tested in preclinical and clinical studies for the treatment of autoimmune diseases, and may also be used to suppress overactive immune responses during viral infection. Source of the original text: Jing et al. SARS-CoV-2 infection causes acute in recovered patients by downregulating CD19 expression in B cells via enhancing B-cell metabolism.Signal Transmission and Targeted Therapy (2021) 6:345; https://doi.org/10.1038/s41392-021-00749-3

